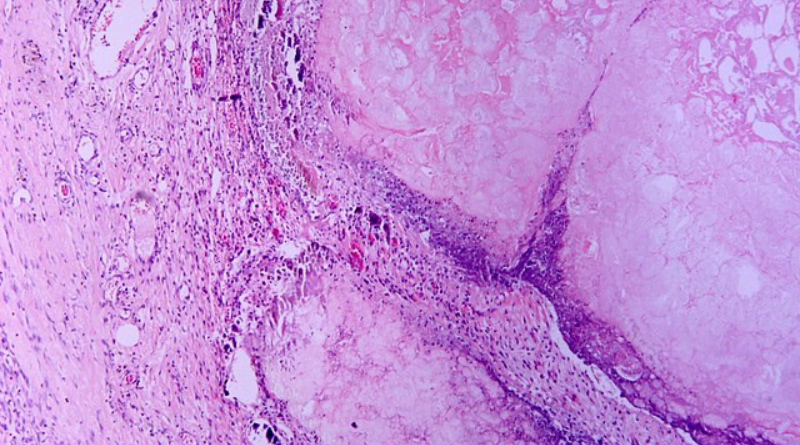
In the realm of internal battles, few are as intense as the searing fire that can ignite within your abdomen, radiating waves of discomfort to your back and chest. Fear not, for this could be a manifestation of pancreatitis, an inflammation of the pancreas, a seemingly modest yet crucial organ nestled behind your stomach.
Despite its modest size—no larger than your hand—the pancreas is a powerhouse, executing dual roles in the body’s intricate symphony:
- Exocrine Mastery: The pancreas crafts digestive enzymes, orchestrating the breakdown of fats, proteins, and carbohydrates in the small intestine via the pancreatic duct.
- Endocrine Wizardry: This multitasking marvel also generates essential hormones, including insulin and glucagon, the maestros of blood sugar regulation.
While the pain may spark panic, understanding the instigators is your beacon through the storm. Two primary culprits often lead the charge:
- Gallstones: Tiny Yet Disruptive: Hardened cholesterol deposits, known as gallstones, can obstruct the pancreatic duct, entangling digestive enzymes and kindling inflammation.
- Alcohol’s Heavy Toll: Excessive alcohol consumption can inflict damage and disrupt the pancreas’s harmonious operation, laying the groundwork for pancreatitis.
Beyond gallstones and alcohol, a variety of factors can join the pancreatic havoc:
- Medications in the Mix: Certain drugs, such as diuretics and steroids, may harbor pancreatic side effects.
- Medical Procedures in the Spotlight: Abdominal surgeries or endoscopic interventions might inadvertently harm the pancreas.
- Triglycerides on the Rise: Elevated levels of blood fats, known as triglycerides, heighten the risk of pancreatitis.
- The Immune Twist: In rare instances, autoimmune diseases like lupus may launch an assault on the pancreas, inciting inflammation.
- Viral Interference: Viruses like mumps, coxsackievirus, and Epstein-Barr can act as unexpected instigators of pancreatitis.
While pain takes the spotlight, heed your body’s subtle cues:
- Abdominal Symphony: Intense abdominal pain, usually starting in the upper middle or left abdomen, may radiate to the back and left shoulder blade.
- Nausea and Vomiting Duet: Digestive upheaval often accompanies the pain, manifesting as nausea and vomiting.
- Fever and Chills Overture: The presence of fever and chills signifies an ongoing infection, a potential aftermath of escalating inflammation.
- Loss of Appetite Interlude: Digestive distress may render the thought of food unappealing, leading to a loss of appetite.
- The Bloating and Tenderness Ensemble: A swollen and tender abdomen becomes part of the distressing symphony.
- Oily or Foul-Smelling Stool: Impaired fat digestion, a consequence of trapped pancreatic enzymes, may result in distinctive stools.
Confronting the Tempest: Navigating Towards Medical Attention
Suspecting pancreatitis demands swift action. Immediate medical attention is your lifeline. Don’t hesitate—call emergency services or head to the nearest hospital.
A thorough examination, focusing on tender areas, sets the stage. Additional investigative acts include:
- Blood Tests: Unraveling the Clues: These tests unveil signs of infection, inflammation, and heightened pancreatic enzymes.
- Abdominal Ultrasound: A painless imaging test may unveil gallstones or pancreatic inflammation.
- CT Scan or MRI: These advanced scans offer a clearer panorama of the pancreas and its surroundings.
- ERCP Drama: Combining endoscopy with X-rays, this procedure explores pancreatic and bile ducts, eliminating any blockages.
Rejoice, for pancreatitis is not invincible. The approach to taming it varies based on severity and overall health:
- Pain Management Prelude: Medications take center stage, alleviating pain while the next steps unfold.
- Intravenous Fluids Interlude: Fluids step in to rehydrate and maintain electrolyte equilibrium.
- Bowel Rest: A Digestive Respite: To foster healing, a hiatus from food may be prescribed, with nutrition delivered through a feeding tube.
- Antibiotics Act: Battling Infection: If infection looms, antibiotics enter the scene to combat the threat.
In cases of gallstone obstruction, ERCP may perform the hero’s role—removing blockages and restoring proper drainage.
While medical interventions play a pivotal role, your active participation is key:
- Culinary Harmony: As you resume eating, focus on a bland, low-fat diet to provide respite for your pancreas.
- Weighty Matters: Maintaining a healthy weight is a linchpin, particularly considering obesity’s role in pancreatitis.
- Spirits and Smoke: If alcohol fueled the fire, a significant reduction or complete cessation is imperative.
- A Smoke-Free Encore: Smoking hampers healing; quitting is a commendable step for pancreas health.
Chronic stress disrupts digestion; combat it through practices like yoga, meditation, or deep breathing.
Addressing the root cause and embracing a wholesome lifestyle can significantly slash the risk of relapses:
- Gallstone Guardianship: For gallstone culprits, consult your doctor about removal options to avert future blockades.
- Diet and Weight: The Pancreatic Custodians: A balanced diet and weight management are custodians of overall pancreatic well-being.
- Moderation’s Shield: Alcohol and Smoke: Mitigate the risk by steering clear of alcohol excess and smoking.
- Chronic Vigilance: Tending to Medical Conditions: Manage underlying conditions like diabetes and hypertriglyceridemia for sustained pancreatic health.
- Rendezvous with Vigilance: Regular Doctor Check-Ups: Scheduled visits allow your doctor to monitor progress and tackle emerging concerns.
Pancreatitis casts a shadow of pain, yet comprehension of its origins, symptoms, and remedies empowers you to navigate the storm. Timely diagnosis and swift treatment hold the keys to a seamless recovery, warding off complications.
Embrace the guidance of your healthcare allies, adopt wellness choices, and prioritize stress resilience. In this journey, you’re not alone. Armed with knowledge, self-care, and proactive health stewardship, you can sail beyond the tempest of pancreatitis into a life of lasting well-being.