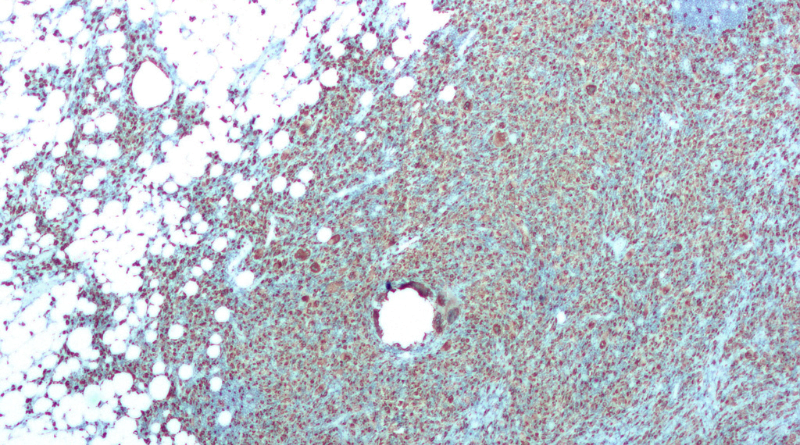
Renal affliction, commonly known as pyelonephritis or a kidney infection, manifests as a grave medical predicament when bacteria originating from diverse sections of the urinary tract, such as the bladder, embark on a journey towards the kidneys, inciting inflammation. This inflammatory response begets distress, elevated body temperature, and additional manifestations of considerable debilitation. If left unattended, pyelonephritis could culminate in severe ramifications, encompassing kidney impairment and the ominous specter of sepsis.
Prevalently, the root cause of pyelonephritis is bacterial intrusion. These microbial agents typically infiltrate the urinary tract through the urethra, the conduit for urine egress. This infiltration may transpire during sexual congress, utilizing contaminated lavatory facilities, or in conjunction with certain medical conditions such as diabetes or compromised immune resilience.
Factors Predisposing to Pyelonephritis
Though pyelonephritis is an affliction that can beset anyone, specific predisposing elements amplify the likelihood of its onset. These encompass:
- Feminine Predilection: Women, endowed with a shorter urethra, face an augmented vulnerability to bacterial ingress, paving the way for affliction to ascend from the bladder to the kidneys.
- Gestation Genesis: The hormonal metamorphosis during pregnancy renders women more susceptible to urinary tract infections, extending to the realm of pyelonephritis.
- Immunological Impairment: Individuals with debilitated immune systems, like those grappling with HIV/AIDS or undergoing chemotherapy, find themselves more susceptible to infections, pyelonephritis included.
- Structural Urinary Anomalies: Anomalies in the structural configuration of the urinary tract, such as obstructions or scarring, elevate the hazard of infections.
- Certain Contraceptive Modalities: The usage of specific contraceptives, like diaphragms and spermicides, heightens the propensity for urinary tract infections, thereby escalating the risk of pyelonephritis.
Identifying the Manifestations of Pyelonephritis
The indications of pyelonephritis are contingent upon the severity of the infection. Nonetheless, some commonplace manifestations encompass:
- Elevated Body Temperature: A fever exceeding 102°F (39°C) is a customary manifestation of pyelonephritis.
- Dolorous Disquiet: Discomfort localized in the lumbar or flank regions is commonly associated with pyelonephritis.
- Frequent Micturition: A heightened urge to urinate, even with meager urine output, stands as another recurrent symptom.
- Ardent Urination: The sensation of pain or burning during the act of urination serves as a poignant indicator of a urinary tract infection.
- Altered Urinary Aspect: Variations in the appearance of urine, be it cloudiness, hematuria, or an offensive odor, signify an underlying infection.
- Nausea and Emesis: Some individuals grappling with pyelonephritis may undergo episodes of nausea and vomiting.
Should the symptoms of pyelonephritis manifest, seeking expeditious medical attention becomes imperative. Timely diagnosis and intervention stand as bulwarks against complications, ensuring a more accelerated convalescence. The attending physician is likely to delve into symptomatology, medical antecedents, and conduct a physical examination. Additionally, urine assays, blood analyses, and imaging diagnostics such as ultrasound or CT scans may be requisitioned to ratify the diagnosis and ascertain the gravity of the infection.
Therapeutic Modalities for Pyelonephritis
The cornerstone of pyelonephritis management rests in antibiotic administration. The choice of antibiotic and the duration of the therapeutic regimen hinge on the specific bacterial culprit and the severity of symptomatic expression. In certain instances, hospitalization may be requisite for intravenous antibiotic dispensation.
Complementary to antibiotic therapy, the healthcare provider may advocate ancillary measures to ameliorate the patient’s well-being, including:
- Repose: Adequate rest is pivotal for the body’s immune system to combat the infection.
- Hydration: Consumption of copious fluids, particularly water, facilitates the expulsion of bacteria from the urinary tract.
- Analgesic Alleviation: Over-the-counter analgesics like ibuprofen or acetaminophen can assuage discomfort and mitigate fever.
While an infallible preventive mechanism against pyelonephritis remains elusive, several prudent measures can diminish the risk:
- Hygienic Vigilance: Regular cleansing of the genital area with mild soap and water, adopting a front-to-back wiping protocol post-urination, and eschewing the use of douches or scented soaps constitute effective barriers against bacterial ingress through the urethra.
- Hydration Imperative: Sustaining optimal hydration levels serves as a deterrent against bacterial colonization in the urinary tract.
- Micturition Regularity: Avoiding prolonged urine retention obviates the opportunity for bacterial proliferation.
- Avoidance of Irritants: Certain substances, such as caffeine, alcohol, and piquant comestibles, possess the potential to irritate the bladder, heightening the vulnerability to infection.
- Incorporation of Cranberry Products: Some studies posit the efficacy of cranberry products in averting urinary tract infections, including pyelonephritis.